Some Known Factual Statements About What Services Are Provided In Acute Care Behavioral Health Units
System that grants access to healthcare to all homeowners or citizens of a nation or region. Universal healthcare (likewise called universal health protection, universal coverage, or universal care) is a health care system in which all homeowners of a particular country or area are ensured access to health care. It is normally organized around providing either all locals or just those who can not afford on their own with either health services or the ways to acquire them, with completion objective of enhancing health results.
Some universal healthcare systems are government-funded, while others are based on a requirement that all citizens purchase personal health insurance coverage. Universal healthcare can be determined by three important measurements: who is covered, what services are covered, and how much of the cost is covered. It is described by the World Health Company as a circumstance where people can access health services without incurring financial hardship.
Among the goals with universal health care is to produce a system of protection which supplies equality of opportunity for individuals to take pleasure in Learn more the highest possible level of health. As part of Sustainable Advancement Goals, United Nations member states have accepted pursue around the world universal health coverage by 2030.
Industrial companies were mandated to provide injury and illness insurance for their low-wage workers, and the system was funded and administered by staff members and employers through "ill funds", which were drawn from deductions in employees' salaries and from companies' contributions. Other nations soon began to do the same. In the UK, the National Insurance Act 1911 provided coverage for main care (however not specialist or healthcare facility care) for wage earners, covering about one-third of the population.
By the 1930s, similar systems existed in essentially all of Western and Central Europe. Japan introduced a staff member health insurance coverage law in 1927, broadening even more upon it in 1935 and 1940. Following the Russian Transformation of 1917, the Soviet Union developed a totally public and central health care system in 1920.
In New Zealand, a universal health care system was developed in a series of steps, from 1939 to 1941. In Australia, the state of Queensland introduced a free public health center system in the 1940s. Following World War II, universal healthcare systems started to be established around the globe.
Some Known Details About How To Take Care Of Your Mental Health
Universal health care was next presented in the Nordic countries of Sweden (1955 ), Iceland (1956 ), Norway (1956 ), Denmark (1961 ), and Finland (1964 ). Universal medical insurance was then introduced in Japan (1961 ), and in Canada through phases, beginning with the province of Saskatchewan in 1962, followed by the rest of Canada from 1968 to 1972.
Italy introduced its Servizio Sanitario Nazionale (National Health Service) in 1978. which of the following is not a result of the commodification of health care?. Universal health insurance was implemented in Australia starting with the Medibank system which led to universal protection under the Medicare system, presented in 1975. From the 1970s to the 2000s, Southern and Western European nations started presenting universal protection, the majority of them building on previous medical insurance programs to cover the entire population.
In addition, universal health protection was presented in some Asian countries, consisting of South Korea (1989 ), Taiwan (1995 ), Israel (1995 ), and Thailand (2001 ). Following the collapse of the Soviet Union, Russia retained and reformed its universal healthcare system, as did other previous Soviet countries and Eastern bloc nations. Beyond the 1990s, lots of nations in Latin America, the Caribbean, Africa, and the Asia-Pacific area, including establishing nations, took actions to bring their populations under universal health coverage, including China which has the largest universal healthcare system worldwide and Brazil's SUS which enhanced coverage up to 80% of the population.
Universal healthcare in a lot of nations has been accomplished by a mixed model of financing. General taxation earnings is the main source of financing, but in numerous countries it is supplemented by particular levies (which may be credited the individual or a company) or with the alternative of private payments (by direct or optional insurance) for services beyond those covered by the public system.
A lot of universal health care systems are moneyed primarily by tax earnings (as in Portugal, Spain, Denmark and Sweden). Some nations, such as Germany, France, and Japan, utilize a multipayer system in which healthcare is moneyed by personal and public contributions. However, much of the non-government financing originates from contributions from employers and workers to controlled non-profit illness funds.
A difference is also made between community and national health care funding. For instance, one model is that the bulk of the healthcare is funded by the municipality, speciality health care is offered and possibly moneyed by a larger entity, such as a municipal co-operation board or the state, and medications are paid for by a state company.
The 25-Second Great post to read Trick For How Does Culture Affect Health Care
Glied from Columbia University discovered that universal healthcare systems are modestly redistributive and that the progressivity of health care financing has limited ramifications for general income inequality. This is normally enforced by means of legislation requiring locals to purchase insurance, but sometimes the government supplies the insurance coverage. In some cases there may be an option of multiple public and private funds supplying a standard service (as in Germany) or often simply a single public fund (as in the Canadian provinces).
In some European nations where personal insurance coverage and universal health care coexist, such as Germany, Belgium and the Netherlands, the issue of unfavorable choice is overcome by utilizing a risk settlement swimming pool to match, as far as possible, the dangers in between funds. Therefore, a fund with a mainly healthy, younger population needs to pay into a payment swimming pool and a fund with an older and mainly less healthy population would get funds from the swimming pool.
Funds are not permitted to pick their policyholders or deny coverage, however they contend primarily on rate and service. In some countries, the basic protection level is set by the federal government and can not be modified. The Republic of Ireland at one time had a "community score" system by VHI, successfully a single-payer or typical threat pool.
That led to foreign insurance provider getting in the Irish market and offering much less pricey health insurance to reasonably healthy segments of the market, which then made greater profits at VHI's expense. The federal government later on reestablished neighborhood rating by a pooling arrangement and a minimum of one primary significant insurance provider, BUPA, withdrew from the Irish market.
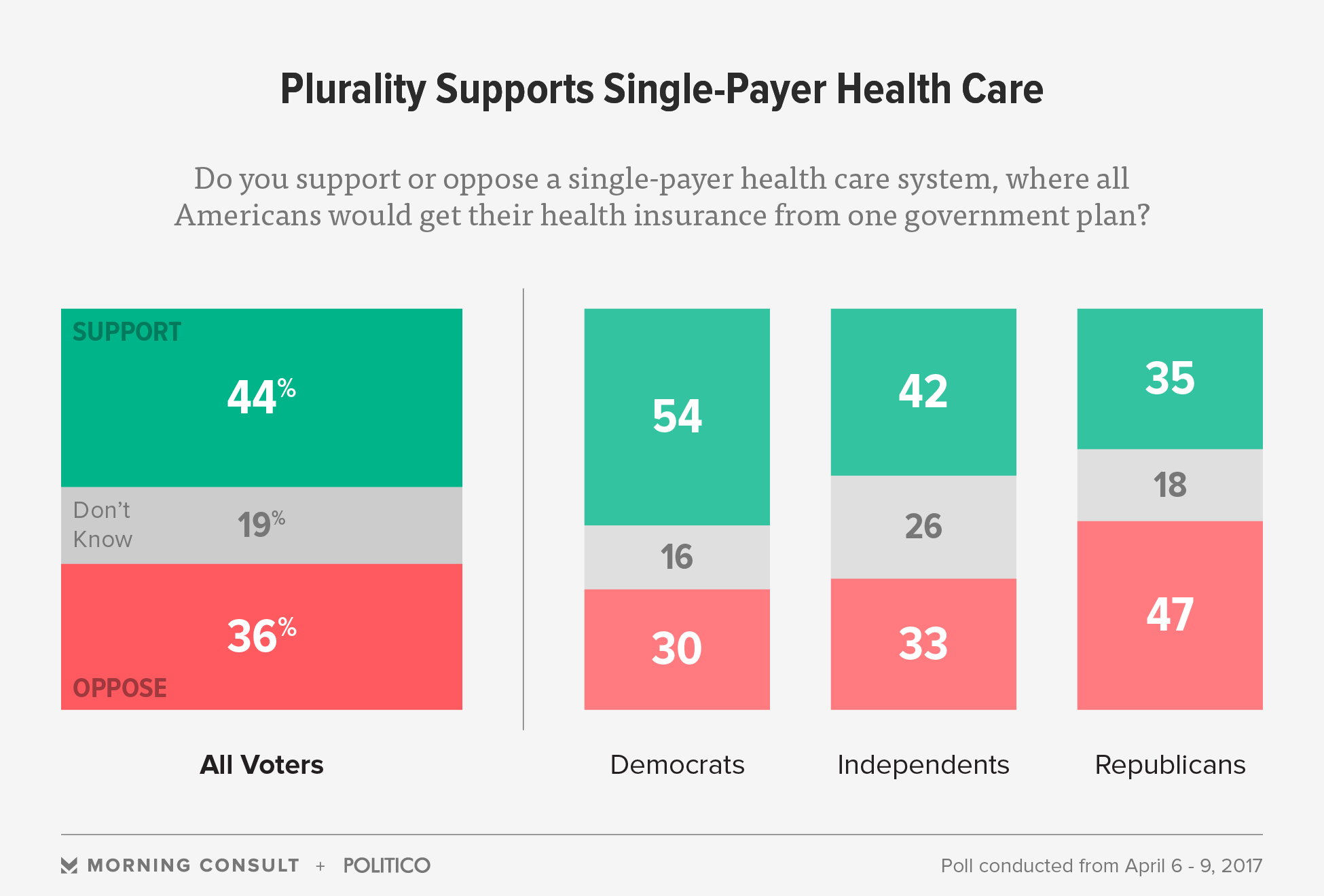
Among the prospective solutions presumed by economists are single-payer systems along with other techniques of guaranteeing that medical insurance is universal, such as by needing all residents to acquire insurance or by limiting the ability of insurance coverage business to reject insurance to individuals or differ cost between people. Single-payer healthcare is a system in which the government, rather than private insurers, pays for all healthcare costs.
" Single-payer" thus explains just the financing system and refers to health care funded by a single public body from a single fund and does not specify the kind of delivery or for whom http://louisonzr132.trexgame.net/why-we-need-to-focus-on-mental-health-care-services-for-beginners medical professionals work. Although the fund holder is usually the state, some kinds of single-payer usage a mixed public-private system.
